GME
UME
CME
OMERAD
Learning Center
Contact Us
Office of Medical Education
2020 Gravier Street
Suite 602
New Orleans, LA 70112
Phone: 504-568-4006
Fax: 504-599-1453
|
|
Graduate Medical Education
Robert Daniels, MD Professorship in Medical Education
On Tuesday, February 24, 2015, after several years hiatus and a request by the Daniels Family, the School of Medicine reinstituted the Robert Daniels, MD Lectureship in Medical Education.
Dr. Daniels retired as the Dean of LSU School of Medicine in 1995. Upon his retirement an endowed professorship in medical education was established by the LSU Medical Alumni Association. Dr. Daniels and his wife, Dr. Vikki Ashley, a PhD psychologist and author, were lifelong and passionate supporters of medical education.
 Pictured: Charles W. Hilton, Jr., MD, Robert S. Daniels Professorship; Stephen Daniels, MD (Son); Zach Daniels, MD(Grandson); Robert J. Nolan, Jr. MD, 2015 Guest Speaker; Allen Daniels (Son); Steve Nelson, MD, Dean of LSU School of Medicine Pictured: Charles W. Hilton, Jr., MD, Robert S. Daniels Professorship; Stephen Daniels, MD (Son); Zach Daniels, MD(Grandson); Robert J. Nolan, Jr. MD, 2015 Guest Speaker; Allen Daniels (Son); Steve Nelson, MD, Dean of LSU School of Medicine
Robert Nolan, Jr., MD; Associate Dean for Graduate Medical Education at the University of Texas Health Sciences Center, San Antonio was the guest lecturer. Dr. Nolan’s presentation on the ACGME Next Accreditation System was an opportunity to facilitate the understanding of the time commitment and financial resources necessary to move GME programs into the next phase of continuous accreditation. In addition, the audience of LSU School of Medicine department heads, program directors, coordinators and chief residents were provided with tools and strategies necessary to assist both departments and training programs in preparation for the new Self Study process and yearly ACGME Review Committee monitoring.
Participants learned more about the criteria and metrics such as aims, Action Plan development and SWOT Analysis to be used for Annual Program Evaluations (APE’s). Dr. Nolan shared UTHSCSA Graduate Medical Education Office ideas and templates they have used in planning for this new accreditation system. The audience was given time to ask questions and present some of their comments and concerns to the group.
Immediately following the Daniels Lecture, program directors and coordinators were offered the opportunity to attend a workshop that focused on the tasks and responsibilities of the Clinical Competency Committees and Program Evaluation Committees in the overall program preparation towards improvement.
Contributing to the Daniels Lectureship fund will ensure this important series continues. To make a donation, please send check payable to: The Foundation for the LSU Health Sciences Center, Attn: Daniels Lecture (Acct# 489070), 2000 Tulane Avenue, 4th Floor - New Orleans, LA 70112.
New Resident Evaluation System
In the coming months the Office of Medical Education will begin offering a new real-time, point-of-care Resident Evaluation system that will be available for use by all GME programs. The system was envisioned by Drs. Kellin Reynolds and Danny Barnhill, from our Obstetrics and Gynecology program. They have had great success in the OB/GYN with the proof of concept evaluation system. They were even invited to ACGME to present and publish their findings: Reynolds, Kellin, & Barnhill, Danny (December 2014) Use of the QR Reader to Provide Real-Time Evaluation of Residents’ Skills Following Surgical Procedures. Journal of Graduate Medical Education.
The Office of Medical Education and its Information Specialists, Christopher Callac and Brett Williams, have been tasked with taking the concept and making it available for all programs that would like to use the evaluation system. Several departments have signed on as early adopters and will be giving all of their faculty and residents ID badges in the coming months. By July we hope to have several departments conducting these quick and easy evaluations. Dr. Barnhill says that when he conducts an evaluation, he works through the evaluation and uses it to create an open dialogue with the resident, the positives and negatives and what the resident can do better next time – immediately after the procedure. Drs. Reynolds and Barnhill have proven how beneficial real-time evaluation can be within the Obstetrics & Gynecology program, and we all look forward to it being successful throughout the School of Medicine.
Coordinator Spotlight
The GME Office recognizes the important work of coordinators across the School of Medicine and our new Coordinator Spotlight will highlight our coordinators who give so much of their time and energy to the position.
In this first Coordinator Spotlight we would like to recognize Susan Wack, pediatric residency coordinator.
GME Coordinator Spotlight
 Name: Susan Wack Name: Susan Wack
Position: Residency Coordinator
Department: Pediatrics
Years of Service: 17 years (the longest of any coordinator!)
What is the favorite part of your job?
I have several favorite parts of my job. Because graduate medical education is constantly evolving, I learn new things all the time, and I am never bored. I also enjoy getting to know each of my residents, and I am happy to be able to make a small difference in their residency training.
What is the most challenging part of your job?
I have a very difficult time delegating tasks.
Hobbies/Interests: home décor projects, travel, plays at The Saenger, baking
Enhancing Quality Improvement for Patients (EQuIP) / Patient Safety
SAVE THE DATE: 3rd Annual Quality Improvement Forum Scheduled for Wednesday, May 27 1-4:30 p.m.
Keynote speech by Dr. Eric Warm (Program Director, Internal Medicine, Univ of Cincinnati College of Medicine)
Please submit abstracts (oral, poster) to Dr. Zee Ali at mali@lsuhsc.edu by March 27th, 2015.
Awards for best oral and poster presentation will be given. Award includes travel support courtesy of the Dean’s Office.
Mark Your Calendar
Important Upcoming Dates
- April 16 - GMEC Meeting – Conference Room 7 at 1:00PM
- April 21 - GME Coordinator Meeting – LEC Room 632 at 10:00AM
- May 21 - GMEC Meeting – Conference Room 7 at 1:00PM
- June 18 - GMEC Meeting – Conference Room 7 at 1:00PM
- June 24 & 25 – Incoming House Officer Pelican Training – MEB MDL Labs at 8:00AM – 5:00PM
- June 26 – Incoming House Officer LSUHSC Training– MEB Lecture Room B at 8:00AM – 5:00PM
- June 30 – Incoming House Officer ILH Training – MEB Lecture Room B at 8:00AM – 5:00PM
Undergraduate Medical Education
John Pelley, PhD
As the Office of Undergraduate Medical Education works aggressively to balance innovative pedagogical practices and strengthen methods of assessment within its curriculum renewal process, this blueprint of curriculum transformation would not be complete without the integration of active learning – a shared experience between lecturer and learner. To maximize the potential of this type of learning strategy, John Pelley, PhD of Texas Tech University Health Sciences Center School of Medicine, presented three distinct faculty development workshops:
- Team-Based Learning
- Techniques for Active Learning
- Question Analysis Groups
Core elements conveyed the emphasis on the accountability of small-group learning with forward-thinking components of application, an exploration of applying logic behind incorrect answers rather than solely focusing on the evidence of correct responses, and the construction of visual concept maps to extend relationships beyond initial content learned. Hosting multiple sessions, 46 faculty members demonstrated their support through attendance and active engagement in this onward march to the rebirth of the School of Medicine’s undergraduate curriculum.
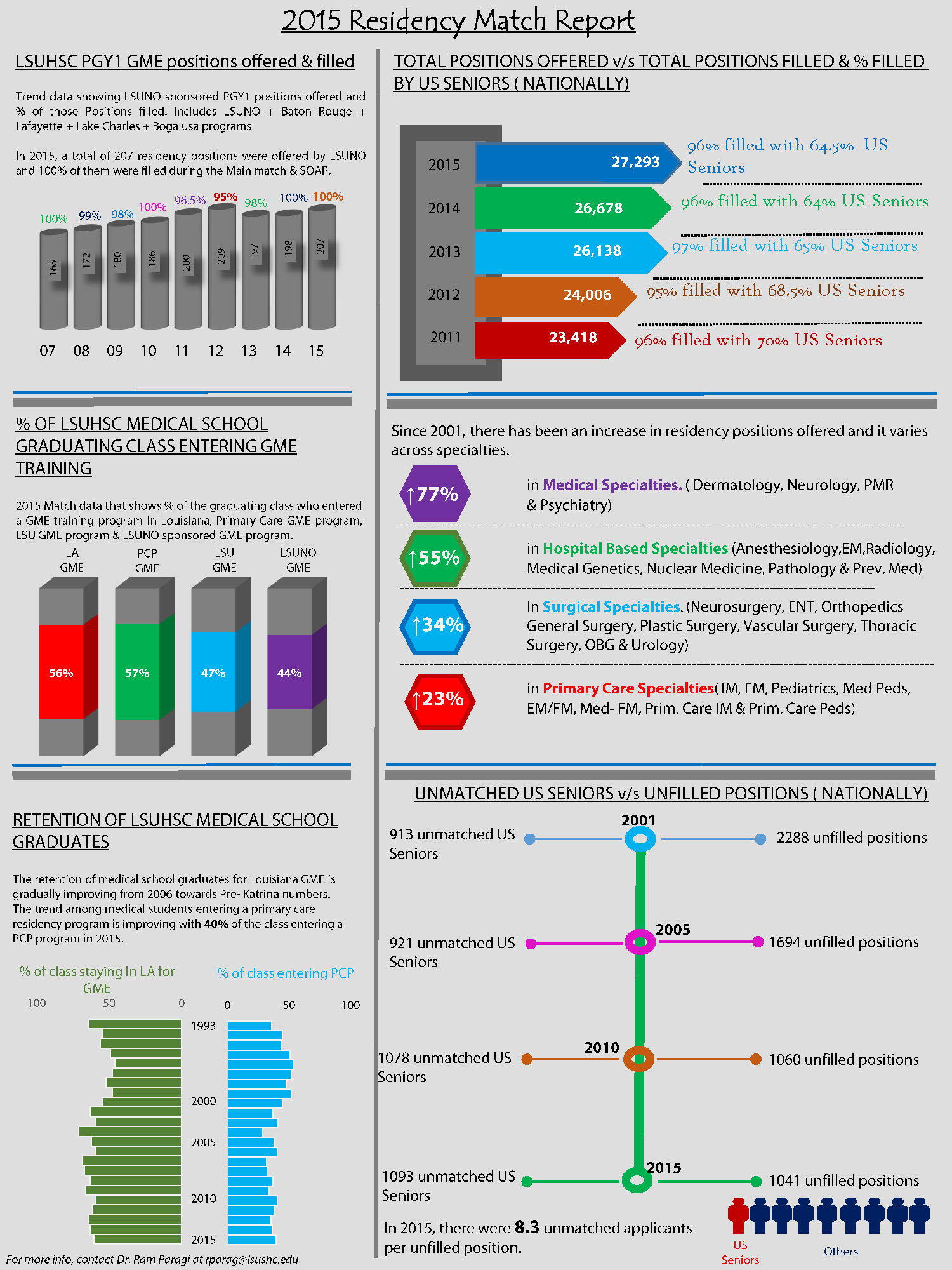
Match Day Infographic
Continuing Medical Education
CME Presents at Alliance for Continuing Education in the Health Professions
Laura Bell, Director of Continuing Medical Education, and Matthew Carlisle, MD, Director of Point-of-Care Simulation presented at the Alliance for Continuing Education in the Health Professions (ACEHP) in Grapevine, Texas in January. The presentation highlighted the use of simulation and hands-on teaching opportunities when designing CME activities. Less than 30% of submissions for the conference were accepted for presentation at ACEHP this year making it the most competitive in the history of the ACEHP.
Evaluating CME for Continuous Improvement
CME providers (for us, the LSU School of Medicine) are required to analyze changes in learners following participation in CME activities and determine whether objectives established in the planning stages have been met. Since the objectives were written as goals for practice change, evaluations measure how participation impacts learners’ practice abilities and strategies, helps to modify their practice, and potentially leads to improved patient outcomes.
Other factors to consider when measuring the effectiveness of an activity are the presentation skills and knowledge of those delivering the content, how well the activity met the learner’s personal educational needs, and whether the audience perceived commercial bias in any aspect of the CME activity, be it in the content, learning space, or behavior of staff and presenters.
There are many ways to perform evaluations, and the format chosen should be customized to yield the most response from a specific target audience. While multiple-choice, true/false and other short-form questions can yield useful information, evaluation should also encourage more detailed responses and open-ended comments for specific and personal feedback from learners on what worked for them and how the activity could improve. A pre and post-test structure is another method a written evaluation can use to quickly highlight changes to a learner’s knowledge base directly following an activity.
Beyond written evaluation, feedback can be obtained other ways, such as an audience response system that asks questions during presentations and gathers immediate response via mobile phones or other devices. A presenter of the activity can also poll the audience by asking for raised hands, having the audience hold up colored cards corresponding to certain answers, or simply pose questions for group discussion. These kinds of informal evaluation methods can be transcribed and measured for analysis much like their written counterparts.
Feedback from learners through evaluation provides vital information on what works and what doesn’t in any educational activity so that planners can engage continuous activity improvement. As the effectiveness of educational interventions is closely measured, the value of future activities increases as they are refined in order to affect the maximum amount changes to practice, and, in turn, improved patient outcomes. As CME activities are designed with the goal of continuous improvement for physicians, evaluation assists in that effort by providing a mechanism for continuous improvement of the education itself.
Office of Medical Education, Research and Development
Dr. Sheila Chauvin, Director, and Dr. Aryn Karpinski, Measurement Consultant, in the OMERAD have been been busy with a number of new and ongoing projects with collaborating faculty. Below are highlights of a number of these developments.
Statewide Simulation Faculty Development Program
With continued funding from the Louisiana Health Works Commission and Board of Regents for 2014-15, this project is well on its way to completion. In this third year of funded activity, a 12-course faculty development program has been developed and implemented statewide in three regions: New Orleans, Lafayette, and Shreveport. This year, the final four courses have been developed and statewide implementation has commenced. New courses address the following needs-based topics determined from a statewide assessment:
- 1) developing inter-professional simulation-based education,
- 2) creating sustainable inter-professional collaborations in simulation,
- 3) project management strategies, and
- 4) practical strategies to enhance success and productivity in professional writing.
Dr. Sheila Chauvin continues to serve as PI for this project, has been leading the course development and train-the-trainer efforts. The four new courses were implemented at LSUHSC-New Orleans on March 3 that were facilitated by Dr. Chauvin, Dr. Matthew Carlisle, and Mr. Daryl Lofaso. Forty-nine faculty members from health professions education programs across the southeast region of the state registered for this first implementation. Participant evaluation feedback was very positive regarding both content and effectiveness of sessions. Minor refinements are being made before the program is repeated April 29 at LSUHSC-Shreveport and on May 18 at the University of Louisiana at Lafayette. Dr. Chauvin will be completing train-the-trainer sessions with faculty members comprising the training teams in Lafayette and Shreveport with whom she will be delivering the courses in these regions. Registration is still open and may be completed by going to https://www.surveymonkey.com/s/VP7XZFX. Seating is limited and on first-come basis by online registration. A statewide oversight team is being established to facilitate continued offerings after this year’s project completion. For more information, please email Dr. Chauvin at schauv@lsuhsc.edu.
Point-of-Care (in situ), Inter-professional, Simulation-based Team Training
Now in its fourth year of funding from the Louisiana Health Works Commission and Board of Regents, Dr. Chauvin (PD/PI) has been collaborating with faculty and leading the expansion of PoC/in situ team training in area hospitals. Dr. Matthew Carlisle, now Director of Point-of-Care Simulation Training in the Learning Center, has been leading the design and implementation of such training with actual health care teams in their own hospital care settings, assisted by Dr. Sergii Rusnak in the Learning Center.
Other faculty with simulation experience and specialization (e.g., Dr. Stacey Holman, Obstetrics and Gynecology) also participate in such simulation-based training to meet priority needs, as indicated by the training needs assessments conducted with hospital leaders. Health professionals have been highly receptive to and positive about this type of training. Several area hospitals have now incorporate inter-professional, simulation-based team training into their regular continuing education programs as a quarterly component. This year’s project also includes exploration of interest and feasibility for expanding training to other regions of Louisiana, specifically the southwest region centered in and around Lafayette and similarly for greater Shreveport area. For more information about this project, please contact either Dr. Chauvin (schauv@lsuhsc.edu) or Dr. Carlisle (mcarl2@lsuhsc.edu).
Envisioning the Future of Simulation-based Education
Dr. Chauvin is working with Dr. Hilton and members of the Learning Center to apply design and strategic thinking principles to envision the future of the Simulation Center and its programs. A small group of Learning Center faculty and staff are engaged in this work and incorporating broad stakeholder input into the design process. Core members working with Drs. Chauvin and Hilton include Laura Bell (Director, CME), Matthew Carlisle, MD (Director, Point of Care Simulation, and Daryl Lofaso (Director, Simulation Operations).
Faculty Development and Scholarly Collaboration
A core mission of the OMERAD is to facilitate faculty development in areas of identified need and interest. Although workshop series were formally a key means of this work, logistics in recent years has resulted such opportunities being reduced and much of this work now conducted predominantly through consultation and collaboration with faculty members individually and in small groups to support innovations and quality in teaching and education and for educational research and scholarship. Drs. Chauvin and Karpinski continue to teach in the core curriculum series for the Department of Pediatrics fellows, faculty, and residents. They also design and deliver customized faculty development programs and session upon request.
In terms of scholarly dissemination, the following occurred during the first quarter of 2015.
Peer-reviewed Conference Presentations:
A poster presentation (Chauvin SW, Karpinski A) and a workshop (Carlisle M, Lofaso D, Chauvin SW, et al.) were well-received at the International Medical Simulation in Healthcare annual conference held January 2015 in New Orleans. January 2015).
Published and In Press Peer-reviewed Manuscripts:
Buttone, L.F., Dicharry, D.Z., Dupont, R.M., Karpinski, A.C., & Trommelen, R.D. (in press). The use of five repetition sit to stand test (FRSTST) to assess fall risk in the assisted living population. Journal of Geriatric Physical Therapy.
Chauvin, S. W. (in press). Applying education theory to simulation-based training and assessment in surgery. K.
Brown & J. Paige (Eds,) Surgical Clinics in North America: Simulation in Surgery Training and Practice (special issue).
Gnilka, P.B., Karpinski, A.C., & Smith, H. (in press). Factor structure of the Counselor Burnout Inventory in a sample of professional school counselors. Measurement and Evaluation in Counseling and Development.
Lepp, A., Barkley, J., & Karpinski, A.C. (2015). The relationship between cell phone use, self-efficacy beliefs, and academic performance in a sample of US college students. SAGE Open, January-March,1-9.
Ulicney, M.L., Ravichandran, S., & Karpinski, A.C. (in press). Implementation of database marketing in the private club industry. International Journal of Hospitality and Tourism Administration.
Manuscript Accepted for Publication:
LaRochelle, J.M., & Karpinski, A.C. (2015). Racial differences in communication apprehension and interprofessional socialization in 4th-year Doctor of Pharmacy students. Manuscript submitted for publication in the American Journal of Pharmaceutical Education.
Manuscript in Review:
Rouster, A.S., Karpinski, A.C., Silver, D., Monagas, J., & Hyman, P.E. (2015). Functional gastrointestinal disorders dominate pediatric gastroenterology outpatient practice. Manuscript submitted for publication in Journal of Pediatric Gastroenterology and Nutrition.
Accepted Book Chapters:
Saha, N., & Karpinski, A.C. (2016). The influence of social media on international students' global life satisfaction and academic performance. In K. Bista & C. Foster (Eds.), International student mobility, services, and policy in higher education. Hershey, PA: IGI Global.
Project Proposals – Extramural Funding:
Harrison-Bernard, L.M. (2015). LSUHSC-NO Postbaccalaureate Research Education Program (PREP) in Biomedical Sciences.” National Institute of General Medical Sciences (NIGMS); NIGMS 1 R25 GM113268-01. Karpinski, A. C. (Senior personnel for program evaluation) and Chauvin, S. W. (Consultant for program evaluation.) (5-year project proposal)
Fournier, S. (2015) HRSA proposal titled, Healthy Teeth, Healthy Communities Project. Chauvin, S. W. (Consultant for faculty development, curriculum development and evaluation, and overall program evaluation). (5-year project proposal)
Area Health Education Center (AHEC) – Southeast Region. (2015) HRSA proposal titled, Geriatrics Workforce Enhancement Project. Chauvin, S. W. (Consultant for faculty development and mentoring). (3-year project proposal).
Miele, L. and Estrada, J. (2015) NIH-NCI proposal titled, Feasibility Studies to Build Collaborative Partnerships in Cancer Research: Training and Education. Chauvin, S. W. (Consultant for curriculum development and evaluation). (P20, 5-year project proposal)
LSUHSC Academy for the Advance of Educational Scholarship
The health sciences center-wide Academy is administratively based in the OMERAD and directed by Dr. Chauvin. To learn more about the Academy, its programs and upcoming events, please go to www.learningcenter.lsuhsc.edu/academy. Interested faculty may submit applications for membership at any time. Reviews are conducted on a quarterly basis. For residents, fellows, doctoral and post-doc, other terminal degree students, membership is available as a Protégé during training, with application and sponsorship by an Academy member in good standing. For more information, please email omerad@lsuhsc.edu or go to the Academy website. You may also enjoy reading the Academy Bulletin, a semi-annual publication that is also available as a PDF from the Academy website. The next issue of the Bulletin will be available in early April 2015.
The Academy is currently undergoing careful review and a design and strategic thinking process is underway to envision its future direction and strategic actions. The Academy Executive Council has begun this work and efforts are underway to gather input from Academy members and the faculty at large. In particular a special session will be held at the upcoming Spring Symposium on Tuesday, April 7 for all interested faculty. A brief questionnaire will be distributed to all LSUHSC faculty to ensure opportunity for providing input. Below are additional details about this event and other upcoming programs and activities.
Spring Symposium and Faculty Development Program
The 2015 program will occur Tuesday, April 7 in the Isidore Cohn, Jr. Learning Center. The Educational Scholarship Day morning program will begin with an open forum for gathering input from all LSUHSC faculty regarding the future of the Academy. The Academy exists to support its members as a professional learning community and to support all faculty members’ development as educators. This is the third strategic thinking process for the Academy and “all is on the table” as we envision the future and how the Academy can best meet the interests and needs of all LSUHSC faculty and its overall education mission. This open session will engage faculty in small and large group facilitated discussions on April 7 from 8:15 – 10:15 a.m. Interested faculty should pre-register by sending an email message to omerad@lsushc.edu, so that planning can be accomplished.
Educational Enhancement Grants (EEG) program
This internal grants program is available to Academy members to support educational and faculty development projects in four categories. Letters of intent have been received and full proposals for 2015-16 projects are due Friday, April 24, 2015.
Docere Fellowship in Health Professions Education
Since 2008, the Academy has offered a two-year fellowship experience to Academy members. Interested members submit applications and are accepted by peer review process. For the 2013-15 Docere Fellowship, three Academy members are nearing completion of the program (June 2015). Some changes are being made in the structure of the Docere Fellowship. Going forward, the Academy will offer two one-year fellowships: one targeting Excellence in Teaching and Learning and the other focused on Educational Research and Scholarship. Details will be included in the new Call for Applications that will disseminated in the week or so. Both fellowship tracks will run July to June. Interested faculty should contact either a member of the Academy Executive Council or Dr. Chauvin.
Upcoming Programs and Opportunities
The annual Back to Basics Summer Teaching Institute will be offered at the end of July. Date and details will be forthcoming soon. The Fall Symposium and Educational Scholarship Day will occur the second week of October. The call for ESD presentation proposals will be distributed in May. The date and details will be distributed in the near future.
Learning Center
Fundamentals of Vascular Surgery Symposium
On February 26 -28, 2015, the LSU School of Medicine Department of Surgery sponsored a "Fundamentals of Vascular Surgery Symposium" for integrated vascular surgery residents from across the country. Led by Malachi Sheahan, MD, the course allowed vascular trainees to perform cadaveric dissections, participate in numerous vascular simulation skills and observe didactic lectures on current practices in the field. In addition to ten LSU physicians, the faculty featured vascular program directors from institutions such as Stanford University, Mayo Clinic and UCLA.
In addition to the teaching portion of the course, all trainees were assessed on the Fundamentals of Vascular Surgery skills. The results of this examination have been compiled since 2012 and are being presented in the plenary session of the Vascular Annual Meeting this summer. This project is expected to set national benchmarks for technical skill development among vascular trainees.
Slaughter Community Charter School toured the learning center on February 13.


Welcome Brett Williams
The Office of Medical Education would like to welcome Brett Williams to our team! Mr. Williams comes to our office with several years of information technology experience, having served as an Information Specialist at the University of New Orleans. He will be responsible for the School of Medicine website and will work with Chris Callac to manage information within the Office of Medical Education. Please join us in welcoming Mr. Williams to the Office of Medical Education.
AHEC
The collaboration of Louisiana Area Health Education Centers (AHEC) and LSU Health Sciences Center kicks off another exciting year for the Primary Care Elective Preceptorship Program – PCE 120! As each year certainly sparks great interests among our rising sophomore medical students to participate in a four-week summer primary care course, no class has ever tipped the scales with 94 students in attendance for an AHEC Interest Luncheon, which was held on December 10, 2014. Soaring numbers also transmitted into the application phase as 57 candidates participated in the interview process. As the notification of placement quickly approaches, we wish all students an unforgettable experience as each specialty and location offers a unique and dynamic opportunity. 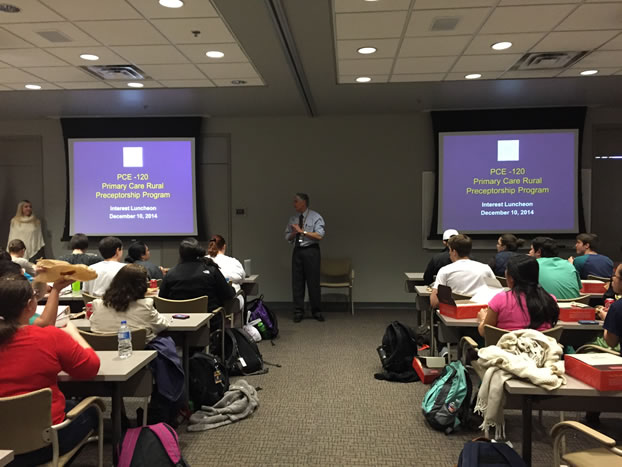
The Office of Undergraduate Medical Education would like to extend a warm welcome to Ms. Elizabeth Sylvest as she transitioned within Central AHEC into a new role as the Health Career Program Coordinator on July 1, 2014. Ms. Sylvest brings a wealth of knowledge of health education that will serve a vital role in the collaboration in our Primary Care Elective Preceptorship Program. Please join us in welcoming Ms. Sylvest aboard!
We would also like to bid farewell to Ms. Nan Ewing of Central AHEC who retired February 3, 2014. Ms. Ewing was an integral part of Central AHEC and the success of PCE 120. We thank her for her time and continued commitment to LSUHSC undergraduate education as she certainly will be missed.
LSU School of Medicine-New Orleans is now on Facebook!
Click the below image to like LSU School of Medicine New Orleans on Facebook.

|

