Pancreatic Neuroendocrine Tumors (PNETs)
Elaine Maggi; Judy S. Crabtree, PhD.
PNETs are a rare form of pancreatic tumor affecting 2-3 people per 100,000. They are a form of neuroendocrine tumor that is generally slow growing and often goes undetected if nonfunctioning. The incidence has been increasing in recent years likely due to better diagnosis techniques and increased awareness.
Pancreatic Biology
The pancreas is an organ that resides in the abdomen and has many important functions. There are two main types of pancreatic tissue, endocrine and exocrine. Exocrine pancreas is responsible for the production of digestive juices that flow through the pancreatic duct into the small intestine. Endocrine pancreas is responsible for the production of hormones, including insulin, which are released into the bloodstream.
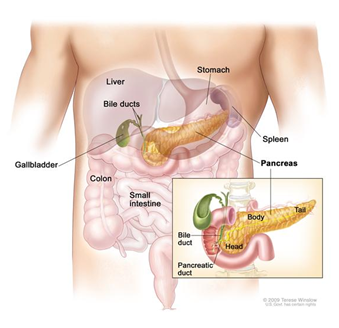
http://www.cancer.gov/images/cdr/live/CDR636528-571.jpg
The endocrine pancreas is composed of different cell types that produce different
types of hormones. The endocrine tissue makes up the Islets of Langerhans, or more
commonly just referred to as islets. The majority of the cells in the islet are beta
cells which are responsible for producing insulin and make up about 80% of the islets.
The other types of cells include:
- Alpha cells which make glucagon (15-20%)
- Delta cells which make somatostatin (3-10%)
- PP cells which producing pancreatic polypeptide (3-5%)
- Epsilon cells which make ghrelin (<1%)
What is a PNET?
Pancreatic neuroendocrine tumors (PNETs), also called pancreatic endocrine tumors (PETs) or islet cell tumors arise out of the endocrine pancreas. Since this is the section of the pancreas that makes and secretes hormones, the tumors can be hormone producing or asymptomatic (they do not product hormones). The hormone producing tumors, also called functional tumors, can be further classified by the type of hormone they produce. Depending on the type of tumor, symptoms may vary.
Hormone secreting tumors (in order from most to least common):
- Insulinoma: This is the most common form of symptomatic tumor and as the name suggests, it produces excess amounts of insulin. The symptom generally associated with insulinoma is dangerously low blood sugar which can lead to confusion, sweating, dizziness, weakness and loss of consciousness. If not treated, low blood sugar can lead to permanent brain damage.
- Gastrinoma: Characterized by the secretion of too much gastrin, these tumors cause diarrhea and peptic ulcers. This is referred to as Zollinger-Ellison syndrome.
- Glucagonoma: This is a type of tumor that produces excess glucagon. It leads to the breakdown of glycogen stores in the liver resulting in high blood sugar, or hyperglycemia. Diabetes can develop from a glucagonoma as well as a skin rash and weight loss. This type of tumor normally is malignant and quickly growing.
- VIPoma : Secretes excess Vasoactive Intestinal Peptide (VIP) which causes Verner-Morrison Syndrome. The most common symptom is severe watery diarrhea, which can be life threatening if dehydration becomes too severe. Many people also experience flushing, or when the face becomes very hot and red.
- Somatostatinoma: These tumors are made up of somatostatin producing cells. Unlike the other hormone producing tumors, symptoms may not occur. If they do, the most common symptoms are gallbladder stones, diabetes, weight loss, and diarrhea.
Non-functioning tumors: PNETs that do not produce excess hormone are called non-functioning tumors. This means they often do not have any symptoms and can go unnoticed for many years. When they become larger some people may have abdominal pain or may feel a lump. These tumors tend to bemalignant because they go longer before diagnosis.
Are PNETs different than pancreatic cancer?
Although PNETs are a type of pancreatic cancer, generally when the term pancreatic cancer is used people are referring to pancreatic carcinoma which is a tumor originating in the exocrine pancreas. This type of tumor is generally more severe than PNETs and has a worse prognosis.
How are PNETs diagnosed?
PNETs can be very difficult to diagnose because they may have no symptoms and grow
very slowly. Many times the symptoms can be misdiagnosed as irritable bowel syndrome
(IBS) or Crohn's disease. In fact, many patients with PNETs are initially diagnosed
with IBS or other disorders, and are the true cause is not found until the tumor has
spread.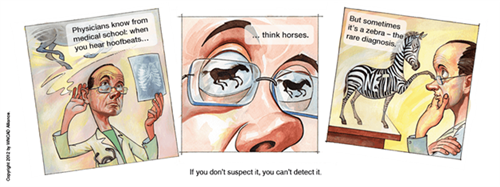
http://netcancerday.org/see-our-zebras-story-so-far
Functional tumors are often detected when a blood test shows elevated levels of the
hormone they are producing. Then the doctor will often order a scan (MRI, ultrasound,
CAT, or other) to see if the location of the tumor can be seen. If the tumor is less
than 1cm in diameter, it can be difficult to see on a scan and other methods will
be tried.
Non-functional tumors are often undiagnosed for many years and generally are found
either when they spread and cause symptoms, or by accident during an unrelated test
such as a chest X-ray before surgery.
Are there risk factors for PNETs?
The only known risk factors for PNETs are a set of hereditary genetic disorders which include: multiple endocrine neoplasia type 1 (MEN1), von Hippel-Lindau (VHL) syndrome, neurofibromatosis (NF) and tuberous sclerosis (TSC). Genetic testing can be done to determine if someone has inherited one of the above hereditary genetic disorders.
The majority of PNETs (90 %) have unknown cause and generally affect people in their 50's and later. There is a slightly higher chance of men developing PNETs, however the differences based on gender are not very large.
How do you treat a PNET?
The most effective treatment for PNETs and the only cure is complete removal of the
tumor before it has the chance to spread. In the event the tumor is not diagnosed
until after metastasis or if it is inoperable due to the location or condition of
the patient, there are medical treatments available to reduce symptoms. Depending
on the type of tumor and whether it is functional or nonfunctional, an oncologist
will treat with different strategies.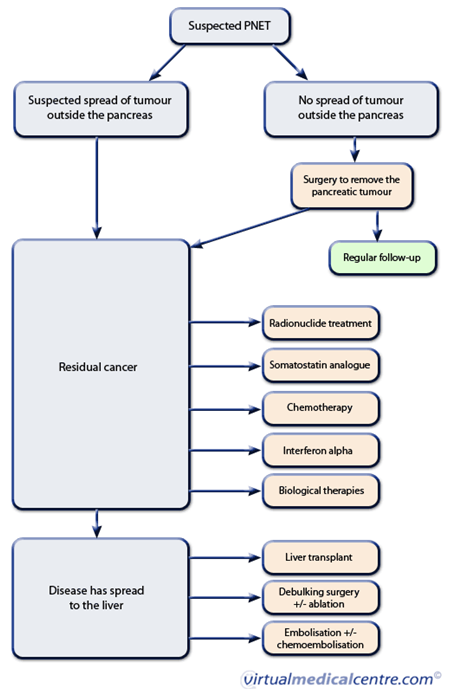
What is the prognosis associated with PNETs?
Given the variation between tumors, time of diagnosis, metastasis, and treatment it
can be difficult to predict the prognosis of PNETs. In general if they are found
and removed before they have metastasized to surrounding tissues, the patients can
be cured.However, 60% of the time the tumors have spread by the time they are diagnosed.
The average survival time after diagnosis for functional tumors is about five years
and this average survival time is decreased to two and a half years for nonfunctional
tumors.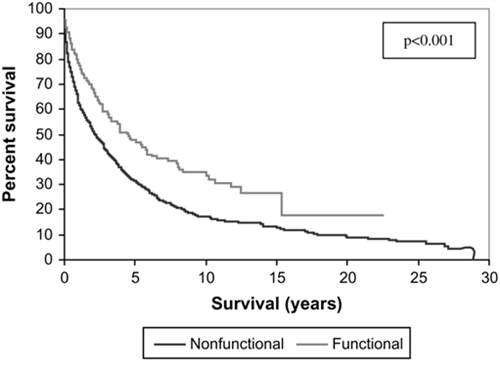
Helpful links:
http://www.cancer.gov/cancertopics/pdq/treatment/isletcell/Patient/page1
http://www.caringforcarcinoid.org/
Sources:
T. R. Halfdanarson, K. G. Rabe, J. Rubin,1 and G. M. Petersen. “Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival”. Ann Oncol. 2008 October; 19(10): 1727-1733.
http://www.cancer.gov/cancertopics/pdq/treatment/isletcell/Patient/page1
http://www.caringforcarcinoid.org/
http://www.virtualmedicalcentre.com/diseases/pancreatic-neuroendocrine-tumour-pnet/942
http://www.cancer.gov/cancertopics/pdq/treatment/isletcell/Patient/page1
