Ongoing Research in the Molina Lab |
|
Alcohol and Traumatic Brain Injury Traumatic brain injury (TBI) is a national healthcare problem, affecting an estimated 1.7 million Americans per year and costing the U.S. economy over $60 billion annually. Mild TBI and concussions are the most common form of TBI, and account for nearly 75% of all TBI related incidents. TBI is a leading cause of morbidity in young adults in the United States. Following mild to moderate TBI, the majority of patients recover physically in weeks to months. However, long term or secondary damage as a result of the mechanical or primary insult, can lead to further damage and has been associated with an increased risk of neurodegenerative disorders later in life. To date, there is no specific treatment for the neurological sequelae of TBI and current therapy is dependent on a patient's symptomology and is primarily focused on physical and psychological rehabilitation. Studies in our lab are focused on determining the processes involved in the long-term effects of TBI, testing new treatments to promote recovery, and examining how alcohol consumption prior to or following TBI can exacerbate the secondary injury processes. Current studies in the lab use the lateral fluid percussion injury in rodent as a model of TBI to investigate neuroinflammation, blood brain barrier dysfunction, glutamate toxicity and immune cell infiltration. |
|
Alcohol and HIV-Associated Neurocognitive Disorder HIV/AIDS affects 34 million people world-wide and up to 50% of these people will develop HIV-associated neurocognitive disorder (HAND). Most people with HAND will experience mild cognitive impairment while others will develop symptoms similar to Alzheimer's or Parkinson's disease. Alcohol abuse by persons living with HIV/AIDS can accelerate the development of HAND. Studies in our lab are focused on understanding how alcohol use/abuse exacerbates neuronal damage during HIV infection, what regions of the brain are most affected, and whether anti-retroviral therapy can prevent these effects. We use a variety of molecular methods to determine changes in gene and protein expression to quantify neuroinflammation, neurotrophic peptides, and immune cell infiltration. |
|
Alcohol HIV and Metabolic Dysfunction There are about 1.15 million persons living with HIV (PLWHA) in the US, with an estimated 35% of PLWHA diagnosed with alcohol use disorders. Increased survival resulting from antiretroviral therapy, has elevated the risk for comorbid conditions due to both chronic alcohol consumption and HIV infection, including myopathy, insulin resistance, prediabetes, and lipodystrophy. Our studies investigate the impact of chronic binge alcohol consumption on progression of HIV disease with particular interest in the alterations in functional skeletal muscle and adipose tissue mass and their critical role as determinants of time to end-stage disease. Integrating pre-clinical and clinical in vivo studies with mechanistic in vitro approaches, our lab is studying the interaction of skeletal muscle and adipose tissue in the progression of metabolic dysfunction due to chronic alcohol abuse in HIV to identify possible targets for therapeutic interventions. Using a number of state-of-the-art molecular techniques, our current studies focus on elucidating the mechanisms of impaired glucose metabolism and protein synthesis in the skeletal muscle, altered adipose tissue phenotype, mitochondrial dysfunction, differentiation potential of satellite cells and adipose-derived stem cells that potentially contributes to the chronic alcohol-mediated metabolic dysfunction. |
|
HIV / AIDS & Alcohol-Related Outcomes; Translational Evidence-Based Interventions Alcohol use disorders (AUD) in PLWHA are associated with increased HIV risk behaviors, suboptimal treatment adherence, potential medication pharmacodynamics and direct negative consequences from alcohol itself. Together, pre-clinical and clinical studies indicate that AUD have detrimental effects on the management of PLWHA, affecting progression of disease. To date, intervention approaches to improve health have not directly or effectively addressed AUD in PLWHA and are untested within primary care settings. Our adapted evidence-based risk reduction intervention has been designed to directly address the information, motivation, and behavioral needs of the target population in order to reduce AUD and improve overall health in PLWHA. Results from our pilot study suggest that the WELL Program is feasible and may contribute to reductions in alcohol consumption as well as an increase in information related to interactions between HIV/AIDS and alcohol use. |
|
Alcohol & Metabolic Comorbidities in PLWHA: Evidence-Driven Interventions ALIVE-Ex
Study According to the Center for Disease Control, an estimated 1.2 million persons were living with HIV at the end of 2013 in the United States and approximately 50% of them had an AIDS diagnosis. Patient mortality has significantly reduced with antiretroviral therapy (ART), and HIV infection has emerged as a chronic disease. The increased survival and aging of people living with HIV/AIDS (PLWHA) on ART is complicated by metabolic comorbidities, including diabetes and obesity. HIV-associated metabolic comorbidities can be further aggravated by hazardous alcohol consumption, which is highly prevalent in PLWHA. Using an animal model, our lab has recently shown that hazardous alcohol consumption and HIV lead to skeletal muscle dysfunction associated with metabolic dysregulation. Skeletal muscle function can be effectively improved by aerobic exercise, thereby reducing the incidence of metabolic cormorbidities. Exercise has also been shown to improve quality of life and mood, increase strength and fitness and lead to better control of blood glucose levels. The ALIVE-Ex Study will extend findings from our parent project, ALIVE, to investigate a sub-population of PLWHA that are at risk of developing diabetes. Preliminary findings from the ALIVE study indicate that 27% of PLWHA have dysglycemia (fasting plasma glucose >94 and < 120mg/dl). Of these, 44% have an AUDIT score of > 5 (measure of hazardous alcohol consumption). In the ALIVE-Ex Study, we will assess whether these individuals have an impaired oral glucose tolerance, skeletal muscle dysregulation, and test the prediction that aerobic exercise will produce an overall improvement in insulin-glucose dynamics. |
 |
 |
 |
 |
|
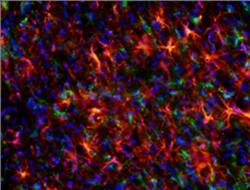
Brain section demonstrating increased astrocyte activation (GFAP - Red) and microglia activation (ED-1 - Green) at 72 hours post-TBI (Nuclei - Blue)
|
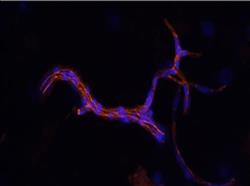
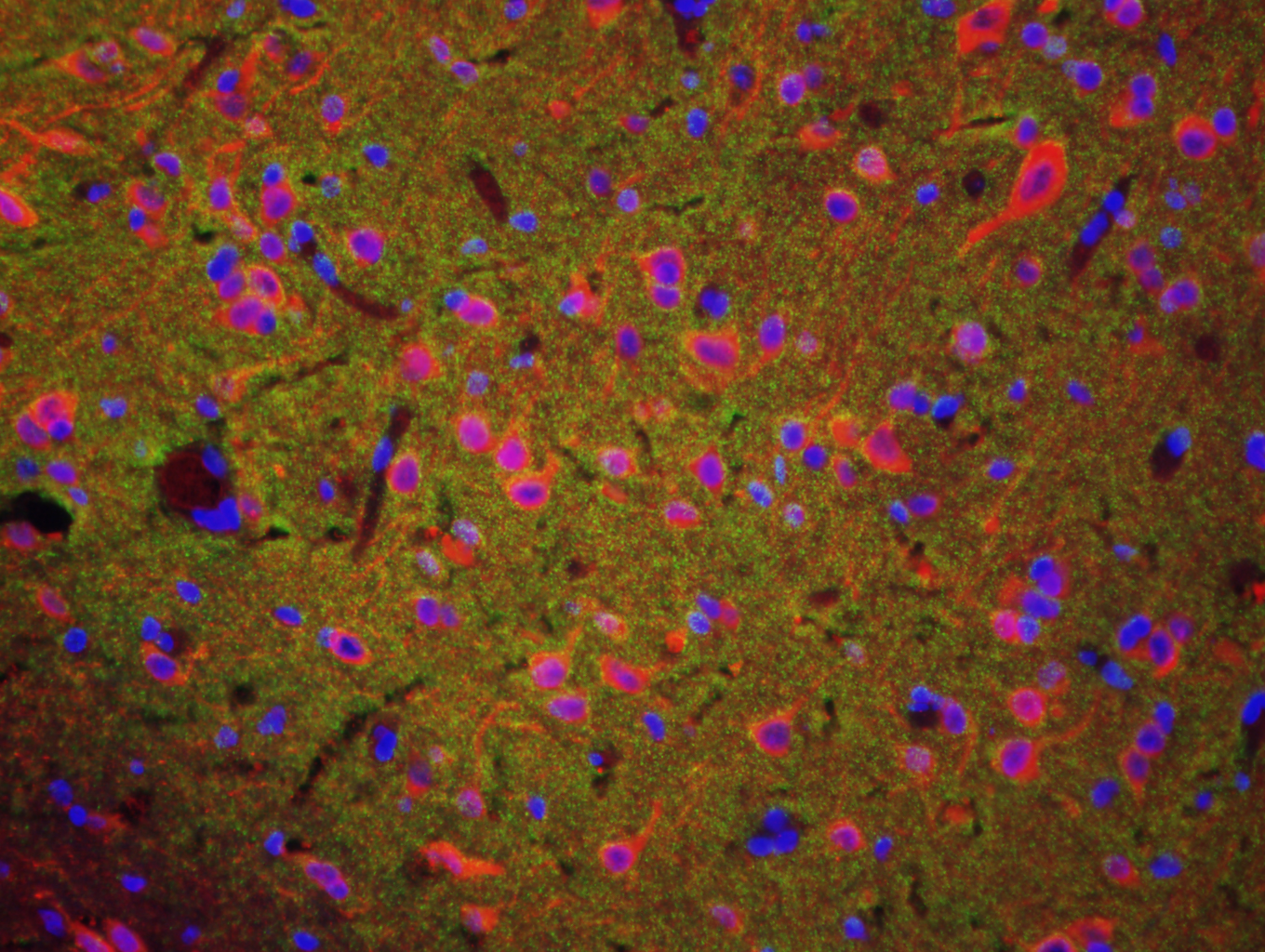
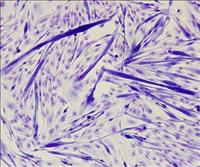
Isolated cerebral microvessel stained for tight junction protein Zona Occludens 1 (Red) TBI (Nuclei - Blue) | Macaque pre-fron tal cortex stained with dendritic marker, MAP2 (red), pre-synaptic terminal marker, synaptophysin (green), and DAPI, (nuclei, blue). | Differentiated primary myoblasts stained with Jenner Giemsa. Myotubes (dark purple) with fused myonuclei, undifferentiated myoblasts (light purple) |
