“From Gene to Function: the Role of the Renin-Angiotensin System in the Regulation of Cardiovascular Function”.
Project 1: ADAM17-mediated ACE2 shedding and neurogenic hypertension. This project was supported by a R01 grant from the National Heart, Lung and Blood Institute (HL093178).
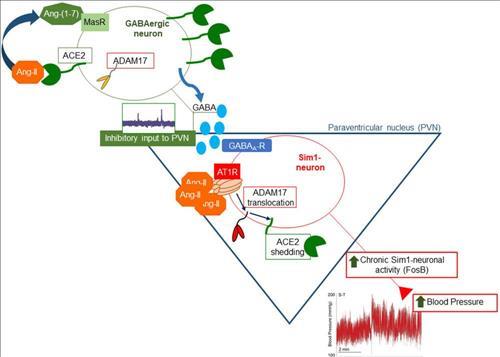
With prevalence higher than 33% in United States, hypertension remains an increasingly important medical and public health issue. Evidence has shown the importance of the brain renin-angiotensin system (RAS) in the maintenance of normal blood pressure (BP) and in the neuro-cardiovascular dysregulation leading to increased sympathetic activity and hypertension. Moreover, clinical trials are currently ongoing to test the efficacy of novel techniques targeting the sympathetic nervous system. Angiotensin (Ang)-II, by means of its type 1 receptor (AT1R), promotes increased sympathetic tone, salt and water reabsorption, vasoconstriction, aldosterone and vasopressin release, all contributing to high BP. ACE2 (angiotensin converting enzyme type 2) is capable of processing Ang-II into the vasodilator peptide Ang-(1-7) and has been identified as a pivotal player in the ACE2/Ang-(1-7)/Mas receptor compensatory axis of the RAS. While numerous overexpression studies have established the benefits of ACE2 in preventing the progression and improving the treatment of hypertension in experimental models, our group and others have shown post-translational impairment of endogenous ACE2 in hypertension. ACE2 shedding, a process by which ACE2 is cleaved from the plasma membrane and secreted in the surrounding milieu, is one of these post-translational mechanisms. The central hypothesis of this proposal is that Ang-II promotes ACE2 shedding, leading to RAS over-activity and hypertension.
Project 2: Consequences of chronic nicotine inhalation for cardiovascular and pulmonary diseases. This is a collaborative project with Dr. Jason Gardner and Dr. Xinping Yue from the department of Physiology at LSUHSC-NO. This project is supported by a R01 grant from the National Heart, Lung and Blood Institute (HL135635).
Even though cigarette smoking is a major risk factor for cardiovascular and pulmonary diseases (CVPD) including hypertension, vascular dysfunction and fibrosis, the direct effects and the molecular mechanisms of nicotine in the pathogenesis of these diseases have not been elucidated. Our data show that cigarette smoke or direct nicotine inhalation disrupts the homeostasis of the RAS in multiple tissues and cell types including the brain, heart and lungs, likely resulting in increased susceptibility to Ang-II-mediated CVPD. Taking advantage of the combined expertise of our multidisciplinary team, we use state-of-the-art molecular, cellular and pharmacological tools combined with unique transgenic and knockout murine models to assess the direct effects of inhaled nicotine on cardiovascular, autonomic and pulmonary functions.
Project 3: Compensatory RAS in type 2 diabetes.
Diabetes Mellitus is affecting 8.3% of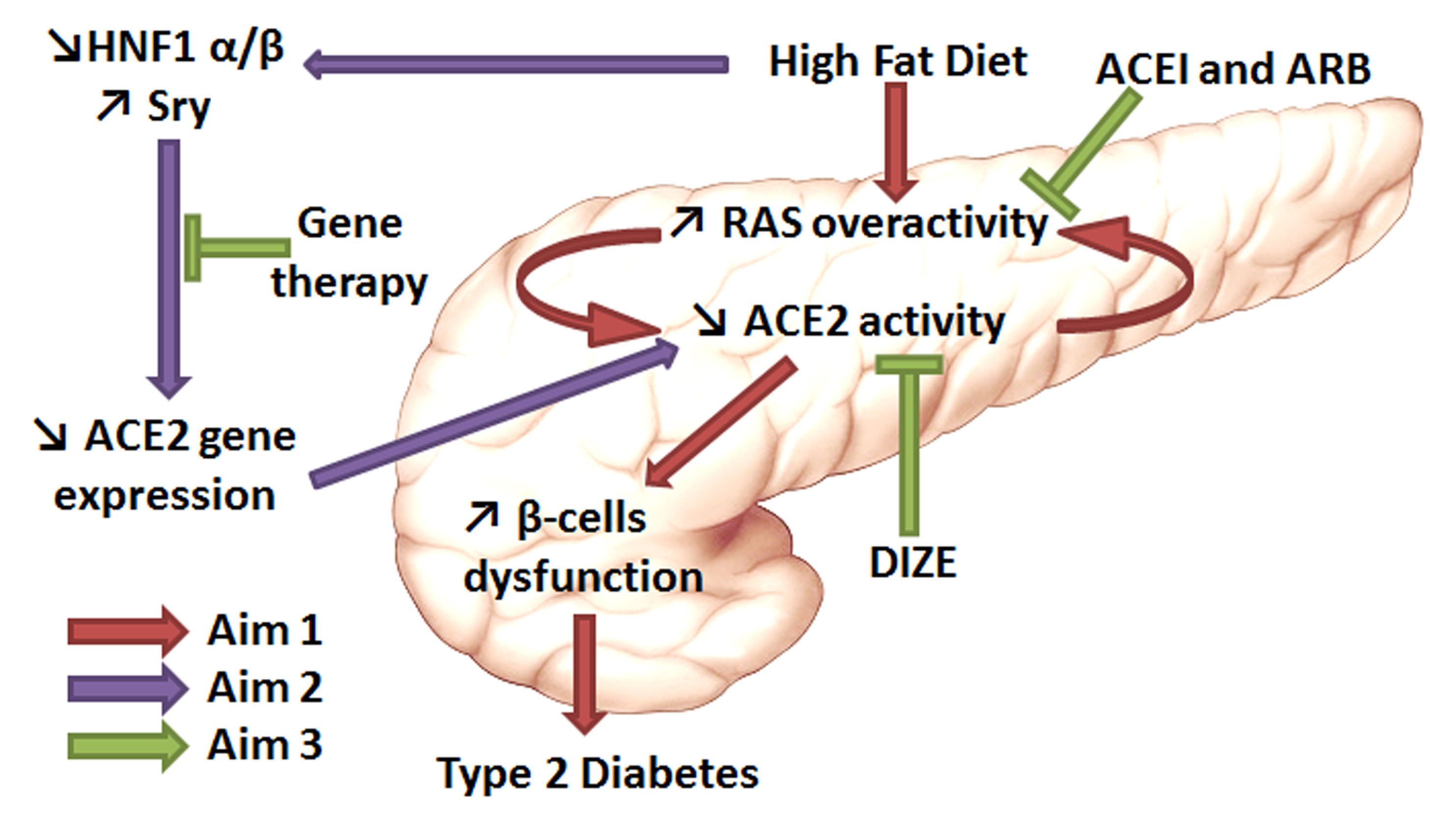 children and adults in United States. With 1.9 million new cases diagnosed in 2010,
diabetes is considered to be an epidemic. In addition, it is estimated that 79 million
people have prediabetes. Therefore, finding new treatments for diabetes is a significant
public health issue. A recent meta-analysis3 shows that renin-angiotensin system (RAS)
blockade with Angiotensin Converting Enzyme (ACE) inhibitors (ACEI) or Angiotensin
(Ang)-II type 1 receptor (AT1R) blockers (ARB) reduces the risk for new-onset Type
2 diabetes Mellitus (T2DM), the most common form of diabetes, in individuals with
hypertension or an elevated risk for cardiovascular events. Moreover, activation of
the RAS potentiates other pathogenic pathways including glucotoxicity, lipotoxicity
and advanced glycation. Accordingly, agents that counteract or block the RAS may have
potential for treatment of T2DM. We previously demonstrated that by promoting the
conversion of Ang-II into the vasodilatory peptide Ang-(1-7), ACE type 2 (ACE2) provides
a compensatory mechanism opposing the overactive RAS in T2DM, thus improving glucose
homeostasis and insulin secretion. However, we also observed that ACE2 expression
and activity are impaired during the development of T2DM. Therefore, the purpose of
this project is to identify mechanisms responsible for ACE2 decline and to implement
strategies to overcome this issue.
children and adults in United States. With 1.9 million new cases diagnosed in 2010,
diabetes is considered to be an epidemic. In addition, it is estimated that 79 million
people have prediabetes. Therefore, finding new treatments for diabetes is a significant
public health issue. A recent meta-analysis3 shows that renin-angiotensin system (RAS)
blockade with Angiotensin Converting Enzyme (ACE) inhibitors (ACEI) or Angiotensin
(Ang)-II type 1 receptor (AT1R) blockers (ARB) reduces the risk for new-onset Type
2 diabetes Mellitus (T2DM), the most common form of diabetes, in individuals with
hypertension or an elevated risk for cardiovascular events. Moreover, activation of
the RAS potentiates other pathogenic pathways including glucotoxicity, lipotoxicity
and advanced glycation. Accordingly, agents that counteract or block the RAS may have
potential for treatment of T2DM. We previously demonstrated that by promoting the
conversion of Ang-II into the vasodilatory peptide Ang-(1-7), ACE type 2 (ACE2) provides
a compensatory mechanism opposing the overactive RAS in T2DM, thus improving glucose
homeostasis and insulin secretion. However, we also observed that ACE2 expression
and activity are impaired during the development of T2DM. Therefore, the purpose of
this project is to identify mechanisms responsible for ACE2 decline and to implement
strategies to overcome this issue.
